We have a new manuscript out in Experimental Eye Research, Natural Immunoglobulin M-based Delivery of a Complement Alternative Pathway Inhibitor in Mouse Models of Retinal Degeneration. (pdf here)
Authors: Balasubramaniam Annamalai, Nathaniel Parsons, Crystal Nicholson, Kusumam Joseph, Beth Coughlin, Xiaofeng Yang, Bryan W. Jones @BWJones, Stephen Tomlinson, and Bärbel Rohrer.
Abstract:
Purpose: Age-related macular degeneration is a slowly progressing disease. Studies have tied disease risk to an overactive complement system. We have previously demonstrated that pathology in two mouse models, the choroidal neovascularization (CNV) model and the smoke-induced ocular pathology (SIOP) model, can be reduced by specifically inhibiting the alternative complement pathway (AP). Here we report on the development of a novel injury-site targeted inhibitor of the alternative pathway, and its characterization in models of retinal degeneration.
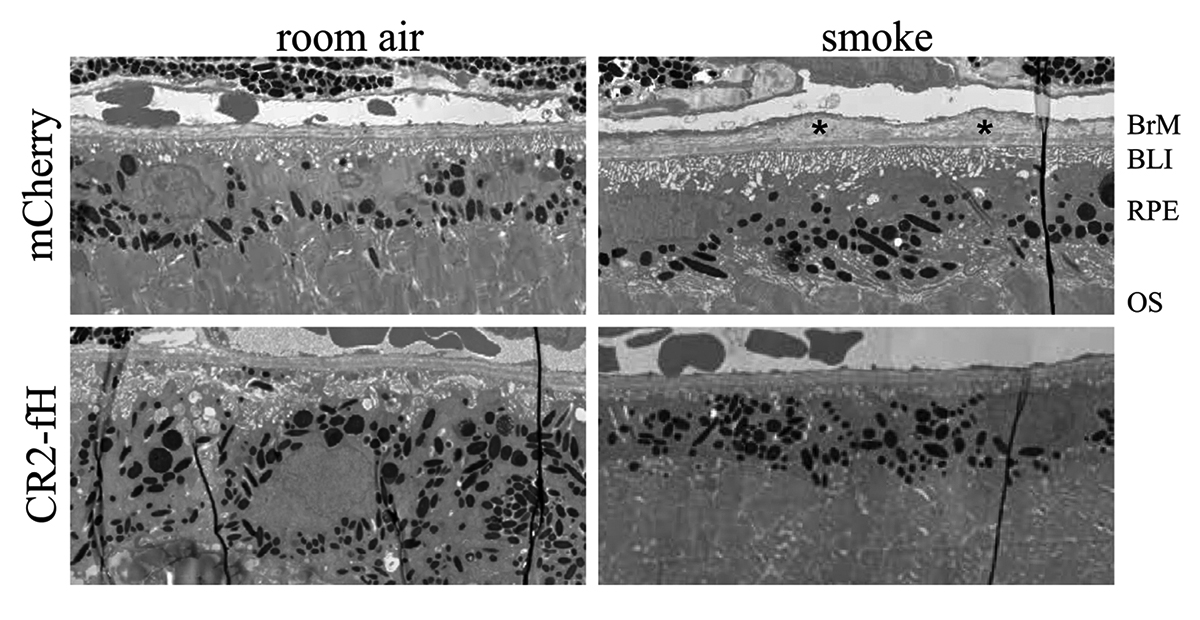
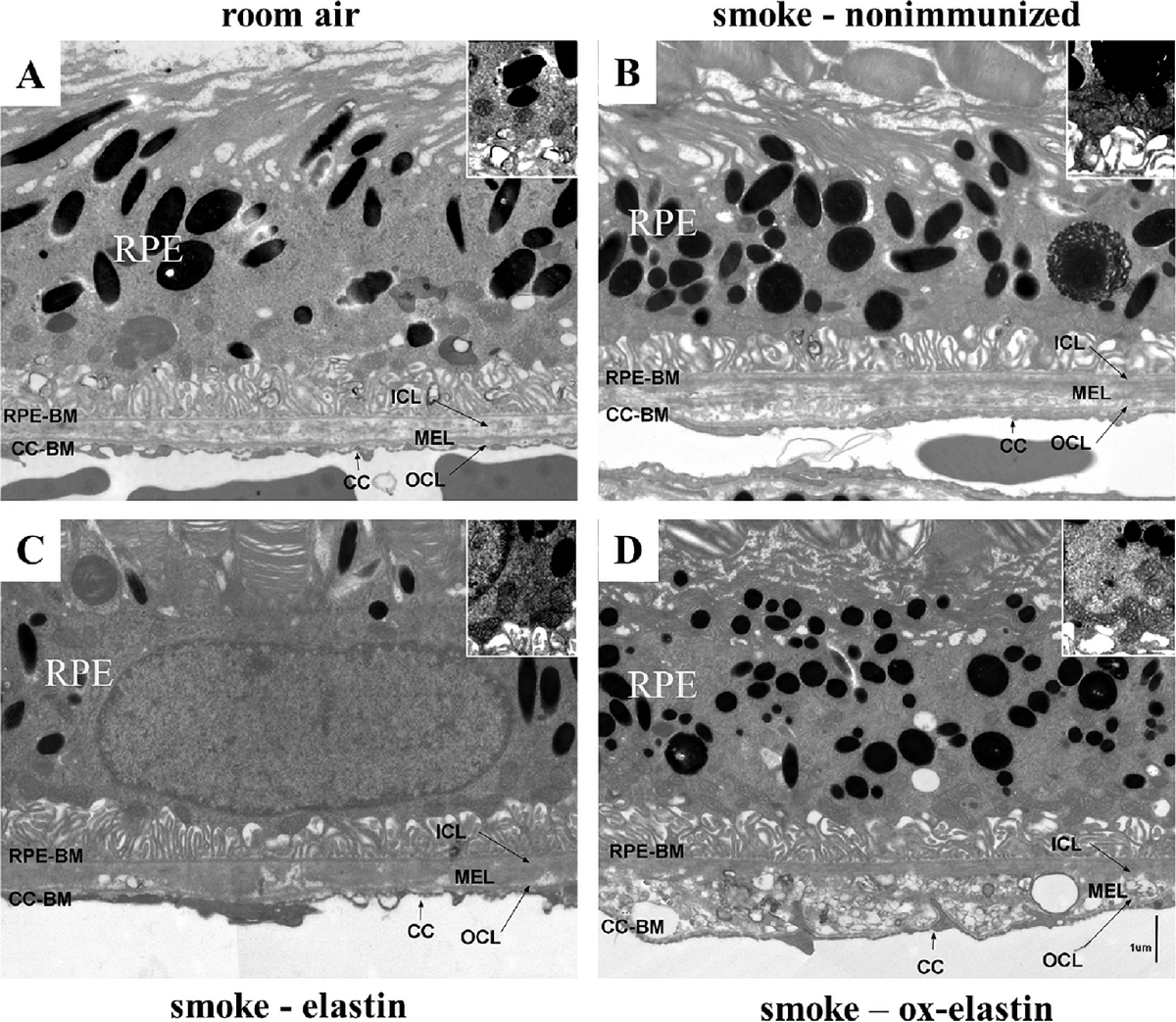
Methods: Expression of the danger associated molecular pattern, a modified annexin IV, in injured ARPE-19 cells was confirmed by immunohistochemistry and complementation assays using B4 IgM mAb. Subsequently, a construct was prepared consisting of B4 single chain antibody (scFv) linked to a fragment of the alternative pathway inhibitor, fH (B4-scFv-fH). ARPE-19 cells stably expressing B4-scFv-fH were microencapsulated and administered intravitreally or subcutaneously into C57BL/6 J mice, followed by CNV induction or smoke exposure. Progression of CNV was analyzed using optical coherence tomography, and SIOP using structure-function analyses. B4-scFv-fH targeting and AP specificity was assessed by Western blot and binding experiments.
Results: B4-scFv-fH was secreted from encapsulated RPE and inhibited complement in RPE monolayers. B4-scFv-fH capsules reduced CNV and SIOP, and western blotting for C3a, C3d, IgM and IgG confirmed a reduction in complement activation and antibody binding in RPE/choroid.
Conclusions: Data supports a role for natural antibodies and neoepitope expression in ocular disease, and describes a novel strategy to target AP-specific complement inhibition to diseased tissue in the eye.
Precis: AMD risk is tied to an overactive complement system, and ocular injury is reduced by alternative pathway (AP) inhibition in experimental models. We developed a novel inhibitor of the AP that targets an injury-specific danger associated molecular pattern, and characterized it in disease models.
Keywords: Alternative pathway inhibitor; Choroidal neovascularization; Complement system; Encapsulated ARPE-19 cells; Natural antibody-mediated targeting; Smoke-induced ocular pathology.