We have a new paper out in the Americal Journal of Ophthalmology, Development of a spatial model of age-related change in the macular ganglion cell layer to predict function from structural changes.
Authors: Janelle Tong, Jack Phu, Sieu K. Khuu, Nayuta Yoshioka, Agnes Y. Choi, Lisa Nivison-Smith, Robert E. Marc, Bryan W. Jones, Rebecca L. Pfeiffer, Michael Kalloniatis, and Barbara Zangerl.
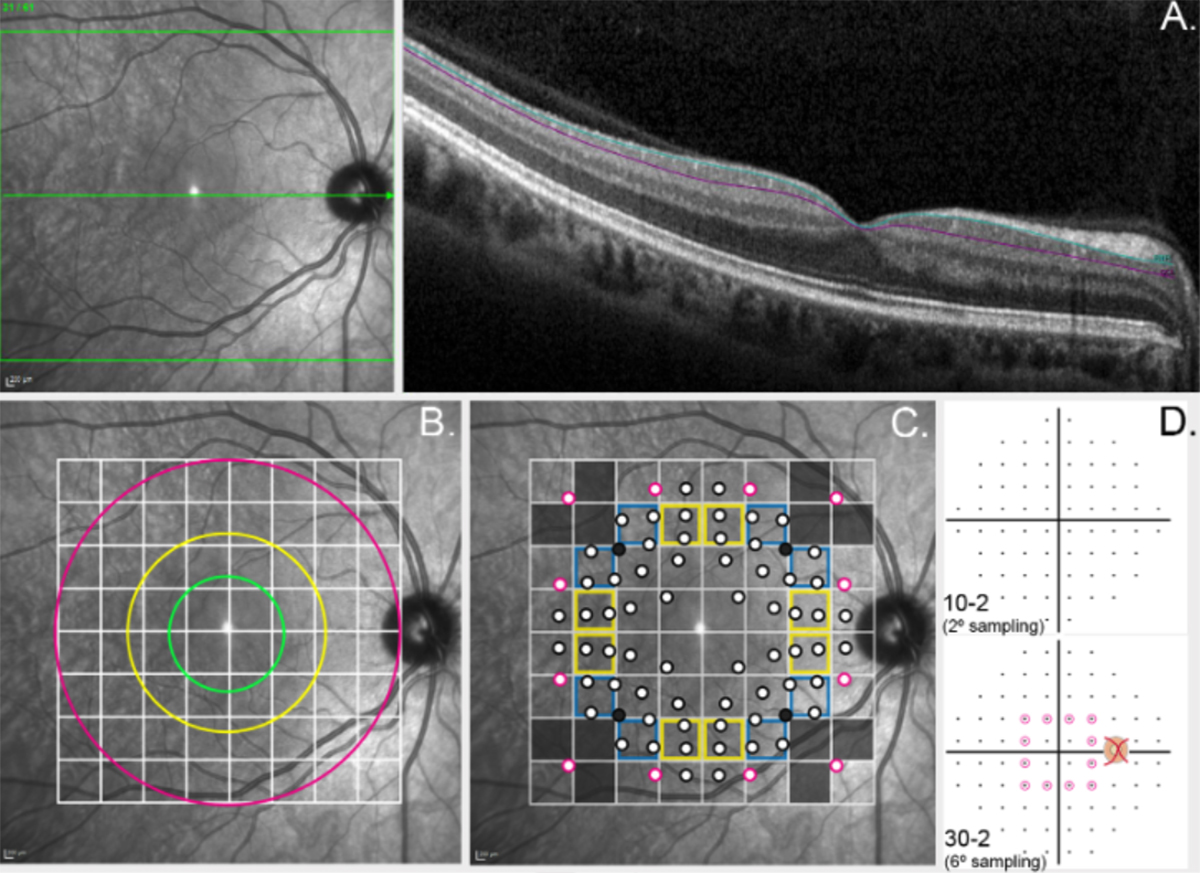
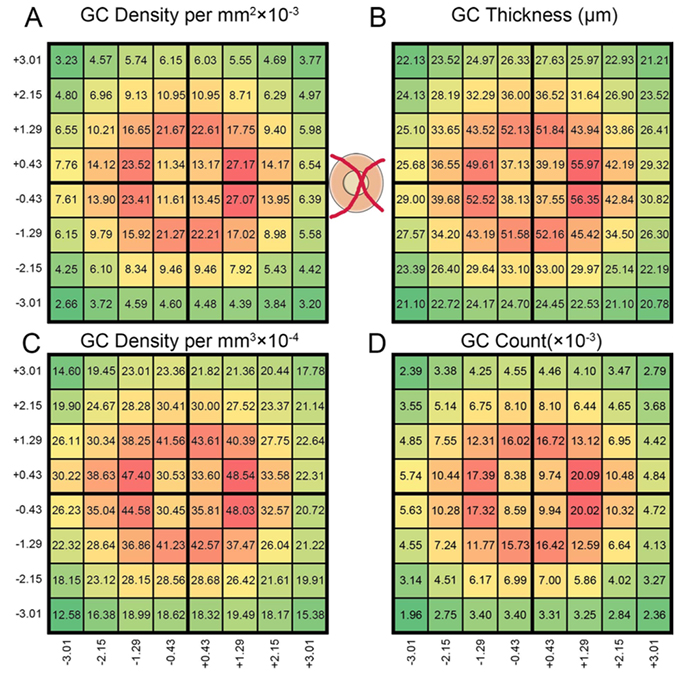
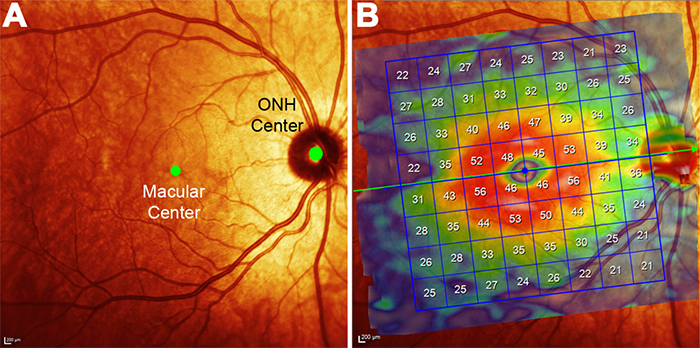
Purpose: To develop location specific models of normal, age-related changes in the macular ganglion cell layer (GCL) from optical coherence tomography (OCT). Using these OCT-derived models, we predicted visual field (VF) sensitivity and compared these results to actual VF sensitivities.
Design: Retrospective cohort study
Methods: Single eyes of 254 normal participants were retrospectively enrolled from the Centre for Eye Health (Sydney, Australia). Macular GCL measurements were obtained using Spectralis OCT. Cluster algorithms were performed to identify spatial patterns demonstrating similar age- related change. Quadratic and linear regression models were subsequently utilized to characterize age-related GCL decline. 40 participants underwent additional testing with Humphrey VFs, and 95% prediction intervals were calculated to measure the predictive ability of structure-function models incorporating cluster-based pooling, age-correction and consideration of spatial summation.
Results: Quadratic GCL regression models provided a superior fit (p = <0.0001-0.0066), establishing that GCL decline commences in the late 30’s across the macula. The equivalent linear rates of GCL decline showed eccentricity-dependent variation (0.13μm/year centrally versus 0.06μm/year peripherally), however average, normalized GCL loss per year was consistent across the 64 macular measurement locations at 0.26%. The 95% prediction intervals describing predicted VF sensitivities were significantly narrower across all cluster- based structure-function models (3.79-4.99dB) compared with models without clustering applied (5.66-6.73dB, p <0.0001).
Conclusions: Combining spatial clustering with age-dependent regression allowed the development of robust models describing GCL changes with age. The resultant superior predictive ability of VF sensitivity from ganglion cell measurements may be applied to future models of disease development to improve detection of early macular GCL pathology.